The most common reason for calf losses in both the beef and
dairy cattle industries is still calving difficulty - the effects of a
difficult birth stretch also into the health and physiology of both the cow and
calf in the weeks following parturition.
Several relationships have been
established that implement
dystocia (difficulty calving) with problems in early
life for calves; contributing to slow or stunted growth or even possibly death.
First of all, the more difficult the
calving the greater the risk of infectious disease; typically, this is
shown by increased rates of diarrhoea and respiratory disease in young calves.
Secondly, the more difficult the calving
the harder it is for the calf to maintain its body temperature following
calving; a decreased temperature can have various implications for general
health and well-being, as well as leading to disease such as hypothermia. The
third relationship observed is that with an increase degree of difficulty
calving, there is a decrease in absorption in protective antibodies by the calf.
Lastly, more difficult calving
procedures lead to increased infertility in the dam. As well as these
in-direct losses, direct losses from death
of the dam or calf must also be added; as well as the delay in resuming to oestrous cycling and reduction in conception shown by those cows or heifers experiencing
dystocia.
In hindsight of these facts, recognition of dystocia comes first from a basic understanding of normal calving.
Pre-Calving Biological Changes
Calving is a complex process. Many
mechanisms have been implicated in affecting the process, but none completely
control it.
As the foetus matures and the uterus
enlarges, the capacity of the placenta
to respond to additional demands of the foetus may not be reached – the placenta
may begin to function less efficiently due to limiting morphologic changes,
which occur during the latter part of pregnancy. These, or other undefined
stimuli, cause foetal stress
reaction. In cattle, this reaction results in an increased production of glucocorticoids such as cortisol and steroid precursors to oestrogen
(i.e. hormones that will eventually lead to the production of oestrogen). These
hormones are released from the foetal
hypothalamo-pituitary adrenal systems (hormone producing parts of the
foetal body). These steroids in turn
enable the foetal-placental unit to produce
oestrogens and prostaglandins. Endometrium layer in the uterus may also
produce prostaglandins. As a result of this process, production of progesterone (which is relatively high due to the
presence of the corpus luteum/yellow body) is decreased, probably at least in part due to the luteolytic effect
of the prostaglandins on the corpus
luteum (i.e. the prostaglandins cause the corpus luteum to regress).
The oestrogens and prostaglandins in turn stimulate maternal release of oxytocin, sensitize the uterus to the effects of oxytocin and cause the cervix to dilate.
The oestrogens and prostaglandins in turn stimulate maternal release of oxytocin, sensitize the uterus to the effects of oxytocin and cause the cervix to dilate.
The uterus is thus released from inhibition by progesterone, which it has been under for the duration of gestation. Following this, it is also made sensitive to the stimulatory effects of prostaglandins and oxytocin and to stimulation by the maternal nervous system.
Uterine muscles, which have increased in contractility in late pregnancy due to stretching, begin to contract regularly as the cervix dilates. When the cervix is fully dilated, the foetal parts are forced into the birth canal. These limbs inside the canal produce pressure points in the vagina, further stimulating the release of oxytocin and initiating the abdominal press (force from the abdomen down onto the uterus and foetus) – this process appears to have a cascade effect (i.e. multiplying effect; this type of process is known as positive feedback. The release of oxytocin causes increased contractions, which in turn produce more oxytocin). The foetus must be delivered or the death of the dam and calf are likely to occur.
This knowledge is useful in order to
understand the bodily processes that are associated with parturition, but
practically speaking, are little help when trying to decipher the signs of
labor and whether or not a cow is ready to calf – or needs intervention to
help.
Signs of Labor
From the practical viewpoint, the
time sequences involved in calving
are more important than the biological
processes. Prediction of time of calving would be of value under certain
conditions, but it is difficult to predict time precisely on the basis of
clinical signs – essentially, all calving situations are different and no
matter how ‘sure’ one can be about clinical signs and previous experiences,
generally speaking there are no set guidelines on how long most processes will take; but there are guidelines on the general order
of the processes.
Practically speaking what this
means is, if a cow starts to show signs of labor and the feet of the calf
appear around 1 hour later, followed by expulsion of the calf in normal
position a further hour later - this should not necessarily be compared to another
cow calving in which the feet do not appear for a long period or less signs of
labor are shown.
Criteria that have been used in
attempts to identify the onset of labor in cattle include changes in body temp, respiration and heart rates, “springing” or relaxation
and enlargement of the vulva, udder changes including enlargement, tenseness
and viscosity of vaginal secretions, relaxation of the sacroiliac ligament (SL)
and dilation of the cervix.
Two of these criteria are the
most reliable forms of estimating
labor initiation – the relaxation of the
sacroiliac ligaments (SL) and cervical
dilation. However, they are difficult to apply on a practical basis.
The first of the two refers to the slackening of the ligaments just above and either side of the tailhead
Relaxation of the SL ligaments can be palpated best by inserting one hand into the rectum and placing the other on the caudal border of the ligament from the outside. Displacement of the ligament can be estimated when pressure is placed against it from the inside. Several days before term, the ligament can be displaced up to 1 inch. This relaxation should not be confused with the progressive relaxation that occurs just before calving, allowing displacement of the ligaments up to 2 inches or more. Successive palpation will help define this stage, which indicates that calving will usually occur within 24 hours.
.
The next indicator, cervical dilation, occurs closer to term and is generally a more reliable indicator of labor. The cervix is part of the cow’s reproductive tract; it acts as a ‘gate’ or ‘wall’ at the entrance to the uterus, which must be ‘open’ (dilated) in order for calving to occur.
Dilation of the cervix begins shortly before calving. It is usually
closed prior to calving; although up to four fingers can be inserted part way
in some cows. Normal dilation preceding calving can be identified by a progressive, conical dilation of the
cervical canal with the apex of the cone towards the internal Os (i.e. the
cervix dilates gradually, from the outside, inwards (towards the uterus)).
When the uterine contractions
begin, which have been stimulated by the foetal
stress reaction, mechanical forces are applied to the internal Os (part of the cervix) and enlargement of the cervical canal proceeds throughout its length.
Once cervical dilation is initiated, calving usually occurs within 24 hours, sometimes in as little
as 6 hours in mature cows. Cervical
dilation is very rapid in most cows after it has opened enough to allow passage
of one hand.
Normal calving is a continuous
process, but for explanatory reasons it can be divided into 3 stages…
Stage 1: The Signs
This stage, lasting 2
– 6 hours (can be longer for heifers), begins with initial labor and
initiation of cervical dilation and ends when the cervix is fully dilated and the calf has entered the birth canal.
The end of stage 1 is marked by the observation of the water sac at the entrance to the vagina (the vulva); an increase in vaginal liquefaction will usually occur before the water bag appears and expulsion of the cervical plug will appear as thick loose strands of mucus from the vulva. The cow may show signs of discomfort by kicking at her belly, becoming restless and often switching between lying and standing out of agitation. Separation from the rest of the herd or residing in the corner of a pen away from the door is often seen.
Stage 1: What is actually happening? I.e. The biology
Each time the uterus contracts, the will cow feel a slight sharp pain which produces her
uneasiness; for heifers, who have never experienced this before, the reaction
to this can be greatly exaggerated so they may show increased signs of
discomfort compared to older cows.
With each uterine
contraction, the attachment of the placenta
to the cow’s uterus (which is very
strongly attached) is becoming increasingly separated. Thus, the oxygen supply to the foetus is
gradually decreasing as the uterine contractions continue – this is because the
placenta is the ‘gateway’ for oxygen to reach the foetus from the dam.
As well as the above process, with each uterine contraction, the cervix is also becoming progressively dilated. When the cervix
is closed, before the onset of stage 1 labor, the cervical plug (mucus blocking
the entrance to the uterus) is present. As the cervix starts to dilate, this
plug is expelled from the vagina and hangs out through the vulva as
white/yellow stringy mucus.
Normally, the first water
sac (chorioallantoic sac) is forced into the dilating cervix and breaks
during stage 1, lubricating the birth canal.
Certain abnormal deliveries are characterized by a failure of
the heifer or cow to progress to stage 2 – by the time the problem is realised,
the calf may already be dead so noting how long a cow is in stage 1 is a good
idea.
Stage 2: Delivering the Calf
This stage begins when the cervix is fully dilated and the second water sac (amniotic sac), plus foetal parts, enter the birth canal further stimulating stronger uterine contractions.
The unbroken water sac is often forced through the vulva
after the cow has been in labor for a short time. The observation of the water sac is probably the most
practical indication to the stockman that the animal is in labor.
When pressure is applied to the inside of the birth canal,
from the calf’s limbs, the abdominal press accompanies its uterine
contractions. The pains of the uterine contractions at this point force the cow
to lie down. The abdominal press is exerted more frequently as labor progresses
until it occurs up to 1-3 times per minute
The calf must enter the birth
canal in a certain position in order to have a normal delivery.
The terms presentation, position and posture
are used to describe how the calf is situated inside the birth canal.
·
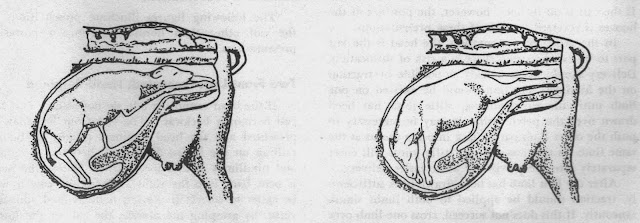
Presentation: refers to whether the calf is coming forwards (anterior) with both front legs and head extended into the birth canal, backwards (posterior) with both hind legs extended into the birth canal (soles of the hooves up and toes pointed down) or transverse with either all four legs in the birth canal or the back of the calf entering the birth canal first.
Both the forwards and backwards presentations are considered normal with forward being the most common. A transverse presentation is never normal.
·
Position: refers to how the calf is
positioned in relation to the cow. If the calf’s back is up towards the cows
back (spine) it is considered to be normal (dorsal). This is the only
position that is considered normal.
It the calf’s back is down on the bottom of the pelvis it is upside down (ventral). The calf may also be on
either of its sides; right-side down or left-side down.
·
Posture: refers to where the calf’s limbs and head are in relation to its body. The limbs and head should be extended into the birth canal, to make the calf long and thin. If the head or one or both of the limbs are ‘bent back’ then the calf is malpositioned and needs to be adjusted prior to delivery.
Summary of terms:
·
Presentation: head first
or tail first?
·
Position: upside
down or normal way up?
·
Posture: legs all
outstretched or some bent back?
The most frequent calf delivery is
an anterior dorsal (this means head
first normal way up) with the leading
limbs outstretched. A backwards presentation is also considered normal but
carries higher risks.
During delivery of the calf, a
series of frequent abdominal presses followed by a short period of rest is
characteristic. The greatest frequency
and force is achieved when the foetal head is being forced through the birth
canal and vulva. Following delivery of the head, a short period of rest may
occur. Strong expulsive forces are required again to push the shoulders and chest through the birth
canal (most people regard this as the most difficult part of the delivery
process).
Sometimes the cow will stop
straining for a short time following delivery of the chest, allowing the rear legs of the calf to rest in the birth
canal – this is not ideal.
At this point, usually the umbilical cord may be compressed shutting off the oxygen supply to the calf from the dam. It is not unusual to observe the calf taking its first breath at this point. This is important to understand because occasionally, at this point, the amniotic sac is still over the head of the calf, and the calf could suffocate if the sac is not broken. However, the sac should only be broken at this point and never before – premature manual sac rupture can lead to decreased lubrication and reduced dilation of the birth canal.
At this point, usually the umbilical cord may be compressed shutting off the oxygen supply to the calf from the dam. It is not unusual to observe the calf taking its first breath at this point. This is important to understand because occasionally, at this point, the amniotic sac is still over the head of the calf, and the calf could suffocate if the sac is not broken. However, the sac should only be broken at this point and never before – premature manual sac rupture can lead to decreased lubrication and reduced dilation of the birth canal.
Delivery of the hips and legs
follows, and is usually uneventful. If the process is normal, the cow should be
able to deliver the calf herself – if assistance is needed, it is known as an
abnormal birth. Assistance can be needed for many reasons. For information on
how to deliver a calf manually and the causes of abnormal calving, click the
following link…
*Insert link here*
*Insert link here*
Stage 3:
Between 2 and 8 hours after the
calf has been delivered, the afterbirth/cleansing/placenta/foetal
membranes should be expelled from the birth canal. If the membranes do not
get pushed out after 8 hours from calving, then this is known as membrane retention. 10 days post
calving the cow will always push out
what is left inside her. By this point, the remnants that are left inside
her will have probably become rotten and produce a foul smelling discharge.
Often retained membranes can lead
to infection of the womb (metritis) and also more systemic infections, as well
as problems with future cycling and
fertility.
Under no circumstances should the membranes be manually removed from the
cow. This can lead to haemorrhage and death, as well as further infection. For
more information on how to deal with membrane retention, visit this specific
blog post… *insert link here*
Often retained membranes can lead to infection of the womb (metritis) and also more systemic infections, as well as problems with future cycling and fertility.












0 comments:
Post a Comment